
Apply for Advancement to Fellowship (FACG).Anticoagulants were restarted and the patient was discharged four days after admission without further event with a GP follow-up scheduled. The patient's Hb recovered to 13.5 g/dL and he became normotensive and euvolaemic. OGD was performed without complication and found no ulcers or bleeding points down to the fourth part of the duodenum. Fluid resuscitation and close observation continued during this period with good urine output and just one further episode of malaena. The patient did not become symptomatic and a blood transfusion was not performed although a group had already been taken. During the period prior to OGD, the patient's blood pressure dropped to 110/70, pulse increased to 95 and Hb decreased to 10.3 g/dL.
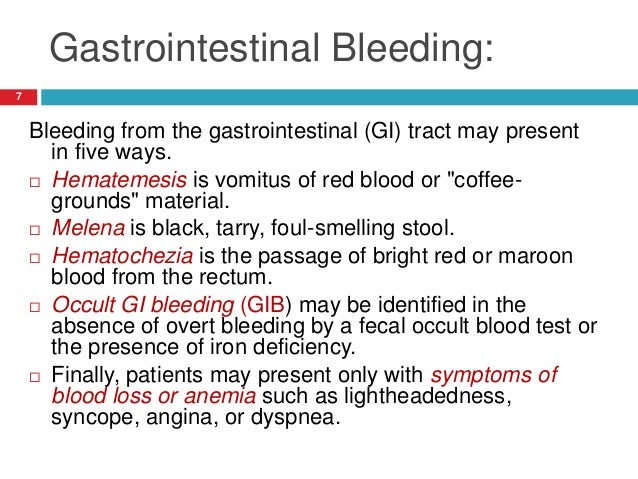
Oesophogastroduodenoscopy (OGD) was scheduled to take place within 72 hours of admission. Fluid and stool charts together with regular observations were initiated. Reversal of warfarin with vitamin K was not deemed necessary. The patient was treated with normal saline IV fluids and his anticoagulants were stopped. The patient's initial Rockall score was thus four which carries a 24.6% risk of mortality. On examination the patient was found to have mild tenderness in the epigastric region. Routine blood tests found that Haemoglobin (Hb) was 12.5 g/dL, with a urea/creatinine ratio >100 and an International Normalised Ratio (INR) of 2.3.
#GI BLEED BLACK STOOL SKIN#
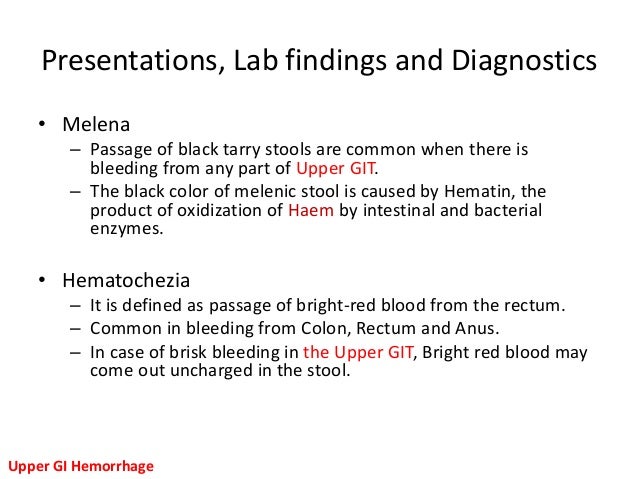
The patient was found to be normotensive at 130/80, but with a postural diastolic drop of 15 mmHg with a pulse of 80, decreased skin turgor, oxygen saturation of 98% on air and a respiratory rate of 16. The patient was a non-smoker, with minimal alcohol intake, a body mass index (BMI) of 25 and with no family history of note. The patient was taking aspirin and warfarin for AF. His past medical history included atrial fibrillation (AF), hypertension, and ischaemic heart disease with a bare metal stent inserted 6 weeks prior to admission in the left anterior descending branch. From that point, the patient had black stools daily with decreasing exercise tolerance and shortness of breath on exertion.

The pain was relieved by eating and settled with simple analgesia and rest. This was similar in nature to the pain from his duodenal ulcers 20 years ago (managed conservatively at the time). Three days previously he had celebrated his birthday when he noted epigastric pain. A retired 80 year old Caucasian man presented to the Accident and Emergency Department complaining of "black stools", increasing shortness of breath, chest tightness and epigastric pain.


 0 kommentar(er)
0 kommentar(er)
